Genomic profiling has allowed physicians to customize treatments for patients with many types of cancer, but bringing this technology to bear against advanced pancreatic cancer has proven to be extremely difficult. OICR’s pancreatic cancer Translational Research Initiative, called PanCuRx, has been conducting a first-of-its-kind clinical trial called COMPASS to evaluate the feasibility of using real time genomic sequencing in pancreatic cancer care. The research team recently reported early results from the trial, which show how they overcame the challenges of genomic profiling specific to pancreatic cancer and gained new insights about the disease.
PanCuRx is focused on improving treatment for pancreatic adenocarcinoma (PDAC), the most common form of pancreatic cancer and the fourth leading cause of cancer death in Canada. The group’s approach centres around understanding the genetics and biology of PDAC to inform the selection of therapies, as well as the development of new treatments.
Kyaw L. Aung, MBBS, PhD, on Pancreatic Cancer: Results From the COMPASS Trial from Harborside on Vimeo.
“Our research, and that of others, has shown that the complexities in effectively treating pancreatic cancer lie at least in the genomic and transcriptional subtypes of the disease,” says Dr. Steven Gallinger, the Leader of PanCuRx and Surgical Oncologist at the Princess Margaret Cancer Centre. “The issue is that right now even advanced techniques such as exome sequencing cannot readily detect these subtypes and inform treatment. Whole genome sequencing and RNA sequencing provide a way to identify these subtypes in patients and use that information to guide treatment.”
Our research, and that of others, has shown that the complexities in effectively treating pancreatic cancer lie at least in the genomic and transcriptional subtypes of the disease
In December 2015, PanCuRx launched a clinical trial called Comprehensive Molecular Characterization of Advanced Ductal Pancreas Adenocarcinoma for Better Treatment Selection: A Prospective Study (COMPASS). The trial is designed to show that the sequencing of pancreatic tumours can be performed in a clinical setting and results delivered within a clinically-relevant timeframe to help guide treatment for individual patients.
Early results from COMPASS, published in Clinical Cancer Research, show that the study has been successful in meeting its primary objective of returning sequencing results within eight weeks, before patients’ first disease assessment CT scan. Genomic results were available to clinicians with a median turnaround time of 35 days. Of the 63 patients included in the initial results, the COMPASS team was able to successfully sequence the genome of 62 and the RNA of 60. As the first study of its kind in pancreatic cancer, to reach this rate of success some challenges needed to be overcome.
the study has been successful in meeting its primary objective of returning sequencing results within eight weeks
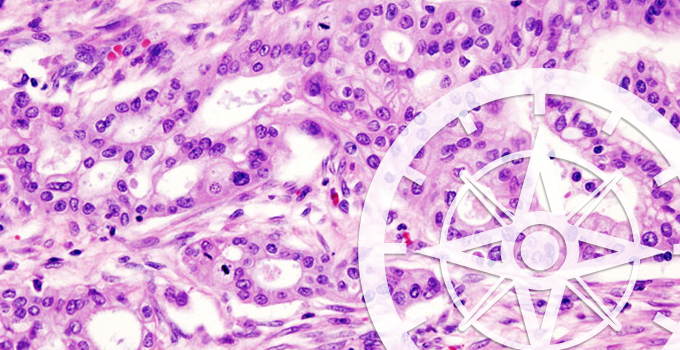
“In pancreatic cancer, we are only able to get small samples from needle biopsies. A further challenge is that these samples exhibit poor cellularity,” says Gallinger. “This is because in a sample there are usually only a few cancer cells mixed into a large stromal landscape. This challenge has stood in the way of sequencing before.” To get the tissue needed for sequencing, the group employed laser-capture microdissection to isolate the cancer cells from the stroma.
In addition to demonstrating the successful implementation of sequencing, the group gained further knowledge about pancreatic cancer subtypes and how these subtypes affect a patient’s response to therapy. The most significant of these findings is the confirmation of an RNA-signature called Moffitt that distinguishes patients with basal or classical subtypes of pancreatic cancer. The COMPASS team was able to show prospectively that patients with the basal subtype typically do not respond to standard chemotherapy.
“Knowing that this subset of patients may not respond to first line chemotherapy means that they may forego these treatments and spare the patient the associated side effects,” says Gallinger. “What’s now needed are new targeted therapies that we can offer these patients. By showing that genome sequencing is possible in pancreatic cancer we hope to spur more interest and investment in repurposing existing drugs or developing the next generation of therapies.”
We want to offer this data to the world. Many basic scientists don’t have access to the high-grade genomic and clinical data that we are capturing under COMPASS
Analyzing a sample for the Moffitt RNA signatures would be difficult to perform in a standard hospital lab, but the study also discovered that RNA expression for a protein called GATA6 could be used as a surrogate Moffitt biomarker in the clinic. Gallinger says that work is already underway to move the test into clinical trials at Princess Margaret Cancer Centre.
Gallinger says that COMPASS will continue to expand to reach more patients and to share results with the research community. “We want to offer this data to the world. Many basic scientists don’t have access to the high-grade genomic and clinical data that we are capturing under COMPASS,” he says. To this end, COMPASS data has been made available to researchers on the European Genome-phenome Archive. This dataset will continue to become even more valuable as COMPASS progresses.
More information
Podcast: COMPASS: Genomic Profiling Could Guide Treatment in Advanced Pancreatic Cancer
