OICR’s Diagnostic Development program is taking two promising breast cancer tests from the lab to the clinic.
The ‘best’ treatments for breast cancer can vary dramatically from patient to patient. Different tumours respond differently to chemotherapies and targeted drugs, and finding the best treatment is about matching a patient’s specific form of cancer to the therapies with the best chance of stopping it.
This tailored approach to oncology is often called ‘precision medicine’ and it’s one of the core objectives of OICR’s Diagnostic Development program. “We develop tools to help understand each patient’s unique cancer so that they can receive the therapies they will benefit most from,” says Dr. Jane Bayani, Co-Director of Diagnostic Development at OICR.
But these tools don’t come easy. It takes a deep understanding of cancer’s underlying biology and a commitment to translating that understanding into clinically useful diagnostic tests.
Bayani and her fellow Co-Director Dr. Melanie Spears have spent nearly a decade developing two promising tests to predict how breast cancer patients will respond to treatment. Buoyed by collaborations across OICR, they have translated their innovations from the early days of biomarker discovery to the cusp of being adopted into the clinic, where they can help inform precision medicine decisions for the one in eight Canadian women who develop breast cancer.
Predicting risk of cancer recurrence
One test looks specifically at hormone receptor positive breast cancer, which accounts for at least 80 per cent of breast cancer diagnoses. For about half of patients, hormone therapy after surgery is enough to keep this type of breast cancer from recurring. But the other half will see cancer return within five to 10 years.
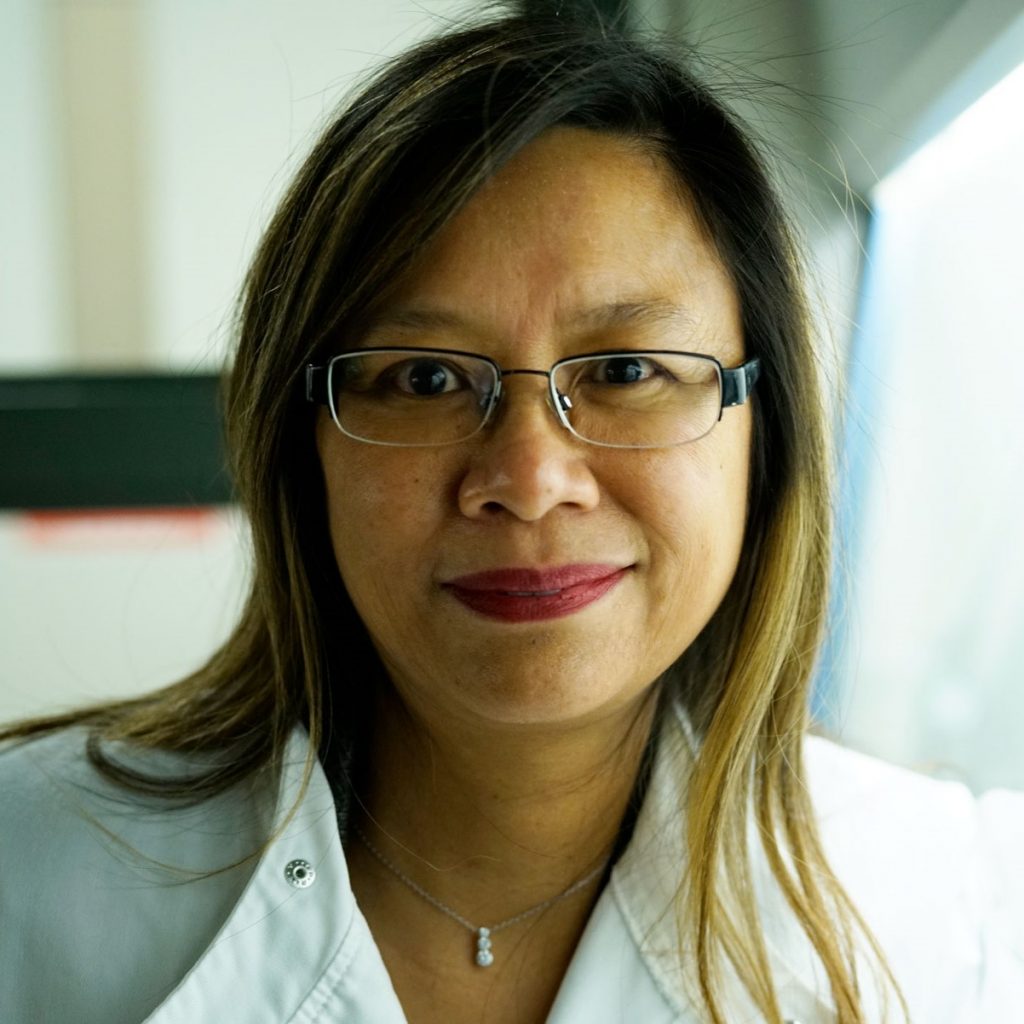
“A significant number will end up dying from the disease,” says Bayani, who has been exploring hormone receptor positive breast cancer since shortly after she joined OICR in 2012.
Back then, there weren’t many reliable ways to predict who might experience a recurrence during or after their initial treatment. This made it tough to determine which patients might benefit from additional drugs like chemotherapy, which could reduce their risk of recurrence.
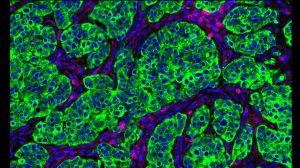
With that in mind, Bayani and Dr. John Bartlett, who was OICR’s Director of Diagnostic Development at the time, set out to look for genetic clues. They identified a signature of 95 genes that seemed to correspond to breast cancer recurrence and developed a corresponding assay. Using a retrospective cohort study, they were able to validate that their 95-gene signature assay can better predict the risk of recurrence in hormone receptor positive breast cancer.
“Patients who are found to be at high risk of recurrence may want to consider chemotherapy, while those identified as low risk can just continue with hormone therapy,” Bayani explains.
But it’s not enough for the test to work in one of OICR’s labs. If this innovation is going to make an impact on patients, it needs to be reproducible at other labs around the world. Working with partners at OICR and external collaborators, Bayani worked to fine tune their discovery, and ultimately created a robust, reproducible assay and are in the process of confirming its clinical utility.
To date, their risk-stratifying test has been patented in Australia and Japan, with a provisional patent in the U.S. and patenting in progress in Canada, China, and Europe. Now, they are working with industry investors to find the best way to make the test widely available. “This is a Canadian discovery that could be disseminated locally, nationally and internationally,” Bayani says. “We’re looking forward to seeing it help patients get the most effective treatment.”
Knowing which cancer treatments work best
Anthracyclines are one of the most effective treatments for women with high-risk breast cancer. But they are also associated with serious side effects like heart failure and the potential to develop leukemia later in life.

“Because of these nasty side effects, we want to be sure that patients who are given anthracyclines will benefit from them,” Spears says.
This led Spears, Bartlett and their collaborators to explore ways to predict a patient’s response to anthracyclines. They worked with OICR’s Adaptive Oncology team to look for genes that were common in different samples of anthracycline-resistant tumours. Through that, they discovered that patients with low expression of histones H2A and H2B, two types of proteins found in DNA chromosomes, and other genes associated with the pathway were more likely to benefit from anthracycline treatment.
From that discovery, Spears, Bartlett and colleagues created what is believed to be the world’s first assay to predict response to anthracyclines and validated it in two separate clinical trials. “I see this assay being used at diagnosis to determine whether a patient should be receiving anthracyclines as part of their chemotherapy regime,” Spears says. “If it shows they won’t benefit from anthracyclines, they can be given a different regime and hopefully not have some of those severe side effects.”
With the test now fully patented the U.S., China, Europe and Canada, Spears and her team are currently exploring licensing options. Thanks to an investment from FACIT, they are also working to validate the test in a third clinical trial, hoping to achieve the highest standard of evidence.
“We want to get this innovation into the clinic,” Spears says. “We want to give clinicians all the evidence they need to be comfortable using the assay in their day-to-day practice.”
Moving toward personalized medicine
With both tests now in the commercialization phase, Spears and Bayani say it’s rewarding to see their projects move from an initial concept all the way toward clinical implementation.
Though the process took several years, they say it was helped by OICR’s commitment to translational research and the infrastructure it has built. “OICR over the past decade has really invested heavily in translational research. Now we’re seeing the fruits in that investment,” Bayani says.
If all goes to plan, OICR’s investment and the tools it is developing will enable a future where all Ontarians have access to diagnostics and treatments tailored to their unique needs.
In the case of the 95-gene signature test, Bayani and her colleagues are hoping to take the next step toward precision medicine.
Working with their industry partners, they are exploring how to link their risk-stratifying test with a targeted sequencing assay used to predict responses to targeted cancer therapies. With the combined knowledge from these two assays, breast cancer patients can be tested for their risk of recurrence, and high-risk patients can be directed to the additional therapies that give them the best chance of survival and quality of life.
“We want to bring that extra information to clinicians and their patients so they can better prioritize targeted treatments,” Bayani says. “That’s what the future of precision medicine is all about.”