Dr. Daniel Schramek never expected to find a major driver for brain tumours in a hidden corner of our DNA.
Then again, he never expected to be studying brain tumours at all.
Schramek’s research focused mainly on the biology of breast, pancreas, and head/neck cancers when he joined Mount Sinai Hospital’s Lunenfeld-Tannenbaum Research Institute (LTRI) in 2015.
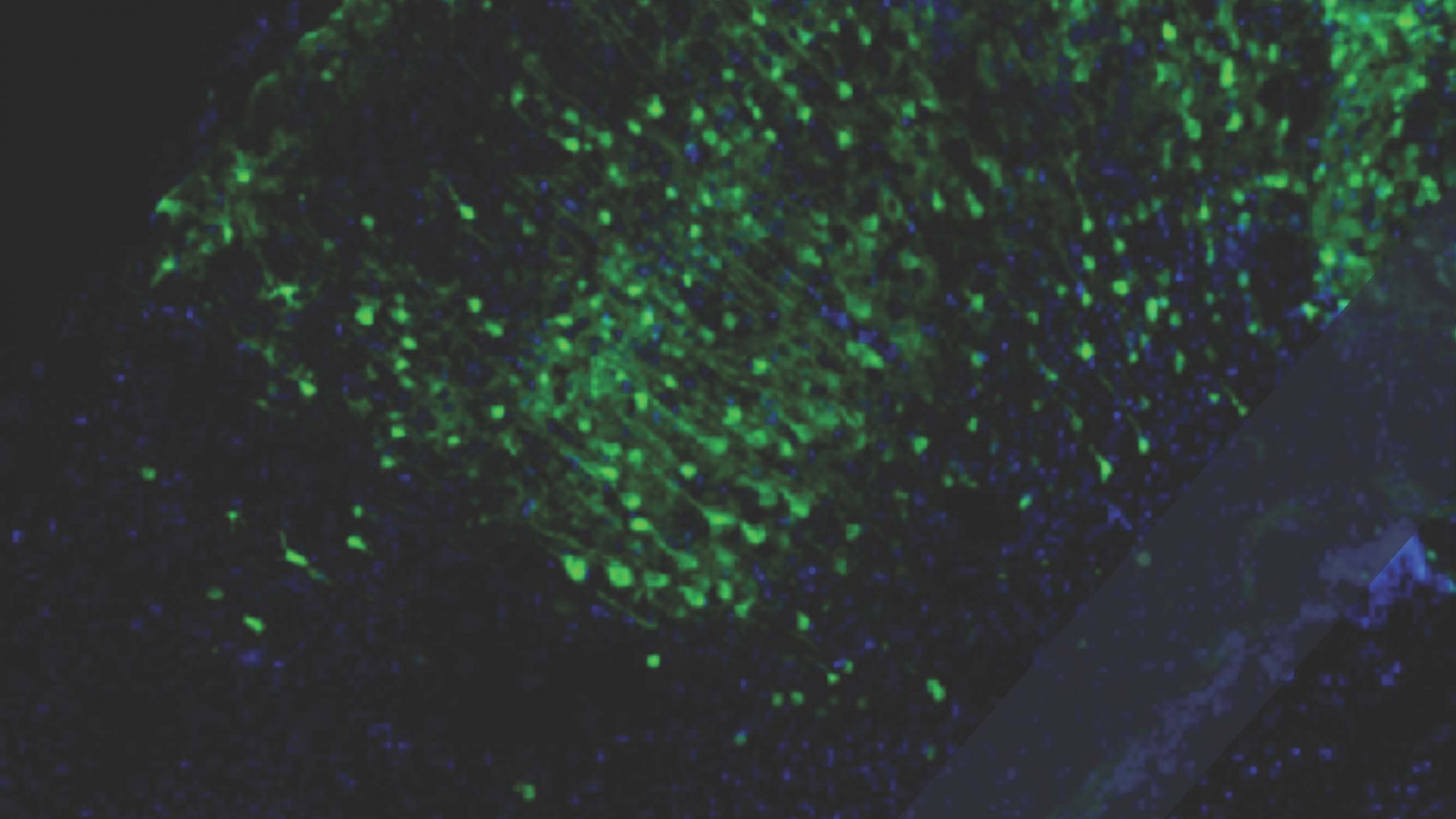
But when a close family member was diagnosed with a low-grade glioma — a brain tumour that arises from the brain’s glial cells — that same year, he decided to read up on it. He found that little was known about how these tumours developed because they were notoriously difficult to model in the lab. So, with support from OICR’s Brain Cancer Translational Research Initiative, he co-led a study to develop the world’s first mouse model for low-grade gliomas.
“It was a very hard experiment and a bit crazy, honestly,” says Schramek, now a Senior Investigator at LTRI and Associate Professor of Molecular Genetics at the University of Toronto. “Maybe the diagnosis in my family was motivation to see it through.”
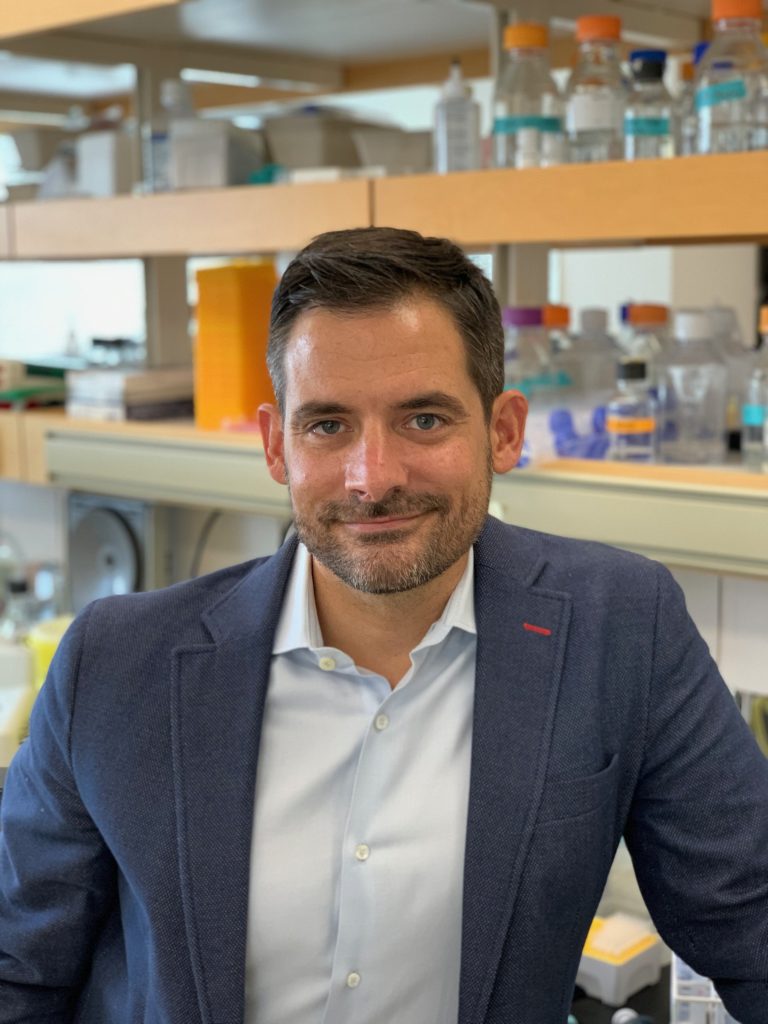
Seven years later, the world-first mouse model is complete, and the study has led to major developments in our understanding of these tumours. As published recently in the journal Science, Schramek and colleagues at LTRI and the Mayo Clinic fine-mapped and characterized a genetic variant (named ‘rs55705857’) that makes people six times more likely to develop low-grade gliomas and causes tumours to develop much earlier.
Their discoveries about the rs55705857 variant being a driver for low-grade gliomas are significant for a few reasons. First is where they found it.
The rs55705857 ‘single nucleodite polymorphism’ is a naturally occurring germline variant, meaning it is present in the DNA of parents’ egg and sperm cells, as opposed to somatic mutations, which arise in other cells after conception and are more commonly associated with cancer. This means that the variant Schramek and colleagues identified, and its implications for cancers, are inherited.
“This is really the first time the inherited component of these tumours has been unraveled,” Schramek says.
It was also surprising to find such a significant cancer-associated variant in a part of the DNA that does not code for proteins. Together with the team at the Mayo Clinic led by Dr. Robert Jenkins, co-senior author of the study, Schramek showed that the variant is in a DNA regulatory region that provides the instructions to fine-tune the expression of essential proteins. However, these regulatory regions are largely understudied and were long considered unimportant.
“We used to think these variants were just noise, but it turns out these seemingly inconsequential variants can actually have a big influence on the likelihood of developing cancer,” Schramek says.
Establishing causality is another important aspect of their findings. It’s one thing to discover that a DNA mutation is linked with cancer risk. But Schramek and colleagues went one step further by demonstrating that this variant actually contributes to causing glial tumours. Their findings suggest that a back-and-forth interaction between germline mutations like rs55705857 and somatic mutations triggers tumour growth.
“Though some cancer-associated mutations are actually very common, they seem to be held in check unless a person has an unfavourable germline set up,” Schramek says.
Findings about rs55705857 are also notable for the mutation’s surprisingly strong association with cancer — a sixfold increase in risk. Most cancer-associated gene mutations only increase risk by one to two times. The only known germline mutation with a comparably high risk is BRCA1, which dramatically increases a woman’s chance of developing breast and ovarian cancer.
Knowledge about BRCA1 and its link to breast cancer has led to targeted screening programs, and Schramek says findings about rs55705857 could spark similar programs for brain cancer. As soon as Schramek found out about the genetic components of low-grade gliomas, he asked his doctors for a brain MRI. Thankfully, the results were negative.
Schramek’s family member underwent surgery that removed most of their brain tumour. The remaining tumour is now dormant, but Schramek says it’s possible it will start growing again in the future. Though low-grade gliomas are less deadly than some other brain tumours, they are difficult to fully remove with surgery. And if they come back, they can evolve into a higher-grade disease.
Schramek and colleagues are now working to understand what causes that progression from low- to high-grade tumours. They are also applying what they learned about the causes of low-grade gliomas to explore therapeutic targets that could give patients more treatment options in the future.
At the moment, Schramek says the biggest implications of this work are for prevention and early detection. Finding brain tumours early is crucial to successfully treating them, and targeted screening could help treat more people earlier and spare others from unnecessary brain surgeries.
“The best cure is to get tumours out early, or even prevent them,” Schramek says. “And I think this new knowledge could be an important step in the right direction.”