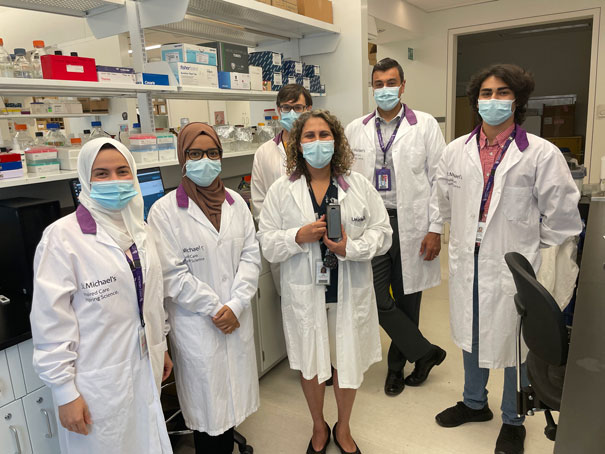
Dr. Rola Saleeb and colleagues harnessed next-generation sequencing to create a test that can identify brain cancer biomarkers for a fraction of the cost of other platforms.
Knowing the subtle differences between cancers, observable only at a molecular level, is increasingly important to treating them.
That’s especially true for gliomas, the most common type of brain cancer. Glioma tumours that have certain genetic mutations respond very differently to one treatment versus another. In fact, glioma’s genetic makeup is so relevant to how it’s treated that guidance from the World Health Organization says it can’t properly be diagnosed without molecular testing.
But the equipment for molecular testing is expensive, and usually only large cancer centres have the money and infrastructure to run it. Samples from patients in smaller, more remote communities must be sent away for molecular testing. That means people with brain tumours can sometimes wait weeks for results before they can even put a name to their cancer — let alone start treating it.
“That time is critical for a cancer patient,” says Dr. Rola Saleeb, Director of the Immunopathology Laboratory at St. Michael’s Hospital (Unity Health) and OICR Clinician Scientist. “People shouldn’t have to wait weeks for information essential to their diagnosis and treatment.”
Saleeb and her colleague Dr. Ramzi Fattouh are working on a way to make molecular testing for cancer faster and more accessible. Collaborating with a research team that includes OICR’s Dr. Jared Simpson and Dr. Harriet Feilotter, and Unity Health Toronto neurosurgeon Dr. Sunit Das, they developed and validated a test — described in the Journal of Molecular Diagnostics — that harnesses new genome sequencing technology to identify genetic variants in less than half the time and for a fraction of the cost of other options.
Their test looks specifically at variants in the IDH gene, one of the most important biomarkers for glioma. The test runs on the nanopore platform, which takes a different approach to sequencing that allows it to decode DNA in real time and can give results in a matter of hours, instead of days.
Scientists have used nanopore throughout the COVID-19 pandemic to sequence to SARS-CoV-2 virus, but this is one of the first times it has been used for cancer. Beyond the speed of sequencing, the biggest advantage of nanopore is that the equipment costs about $1,000 USD and is no bigger than a mobile phone. Standard DNA sequencers can cost hundreds of thousands of dollars and are much larger, often requiring a special room to house and operate them.
“This type of work lowers the barrier for labs and clinics to benefit from the very rapid pace of cancer genomic discoveries,” says Dr. Simpson, an OICR-based investigator specializing in computational biology.
Simpson’s lab worked with Saleeb’s team to develop the software to analyze and interpret the sequencing data for their test.
To validate the test, Saleeb and colleagues sequenced 66 patient samples and found that it met every benchmark for clinical use.
“We proved the technology is as accurate as the other platforms,” she says. “This is proof of concept that it can be implemented in a clinical laboratory.”
Saleeb says the test is easy to reproduce, and she encourages labs to read the details of the journal article and contact her if they want advice on implementing it. She is also working with PhD student Mashiat Mimosa to expand the test to look for other genetic variants relevant to glioma. In time, they would like to create an all-in-one glioma biomarker test on the nanopore platform.
But glioma is just the starting point, and Saleeb says similar tests could be developed for other cancers. With oncology entering a “molecular era” where DNA sequencing will likely become part of how all cancer are diagnosed, she says that accessible and affordable molecular testing will become even more important.
“I want to get molecular testing in every laboratory, so that people everywhere can be empowered with the information they need to get the best possible cancer care,” Saleeb says.