An OICR Imaging project has developed a 3D ultrasound system that provides real-time feedback on the best placement of thermal ablation applicators.
To fully destroy a liver tumour, Dr. Derek Cool must guide his thermal ablation applicator needle into a patient’s abdomen, avoiding vital organs and blood vessels, to the exact centre point of a tumour.
“If I’m off centre by just a couple of millimetres, the ablation might not cover the entire tumour and the patient won’t get a complete treatment,” says Cool, an Interventional Radiologist at London Health Sciences Centre and Assistant Professor in Western University’s Department of Medical Imaging.

Thermal ablation is a procedure where heat is used to kill cancer tissue. It’s highly effective, less invasive than traditional surgery and used around the world, but outcomes vary because of the challenge of placing the applicator needle so precisely. With such small margins for error, the procedure takes coordination and dexterity from the physician and a clear view of the tumour, the needle and the surrounding tissue.
That view is usually provided by one of two imaging tools — ultrasound or CT scan — but both have their limitations. Ultrasound delivers real-time images, but only on a 2D plane. CT scans provide a more wholesome view, but not in real-time. And access to CT is limited, especially in smaller healthcare centres and in the developing world.
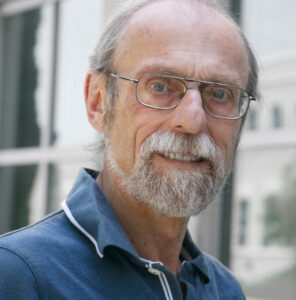
Cool wanted to create a more accessible tool to make thermal ablations for liver cancer more accurate, so he teamed up with OICR’s Director of Imaging Dr. Aaron Fenster to develop a 3D ultrasound guidance system and test it in an ongoing clinical trial.
The system they developed is compatible with standard ultrasound equipment, making it a potential low-cost upgrade for healthcare organizations. It works by attaching a 2D ultrasound transducer to a robotic arm that moves it around and takes images at different angles. Those 2D images are synthesized by a computer program that generates a 3D image.
“Ideally, our system provides a 3D view of the whole tumour and allows the procedure to be done entirely with ultrasound, without having to occupy a CT scanner,” Fenster says.

The first half of their trial focused on feasibility. The 20 ablation procedures performed by Cool and his interventional radiology colleagues were guided by 2D ultrasound, and 3D images were collected to be reviewed afterward. From these first 20 patients, they found that it was easy to incorporate the 3D ultrasound system into the ablation procedure and the 3D images effectively showed the needle position within the tumour.
The 3D ultrasound data from these early patients showed that the needle insertion with 2D US was accurate, yet improvements in the needle position was still possible. They worked with colleagues to develop software that uses 3D ultrasound data to analyze the position of the applicator needle, predict how likely a full ablation is from that position, and provide guidance on where to move the applicator for a more complete ablation. In a recent IEEE Transactions on Medical Imaging paper, they reported that feedback from their software could have improved needle placement in eight of 14 procedures.
“The physician needs to know when they start the ablation if it will be successful,” Fenster says. “Our software tells them whether the needle is too deep or too shallow, or needs to move up, down, left or right in order to be successful.”
In the next phase of their trial, Cool aims to use 3D ultrasound as part of the procedure to confirm needle positioning and suggest adjustments, which is how he thinks it could be most helpful as part of a radiologist’s workflow. Though he has performed more than 200 successful ablations, he says he often finds himself wanting another angle to pinpoint the centre of the tumour.
“The 3D ultrasound is going to improve our ability to assess where our applicators are and confirm if we’re going to get full tumour coverage,” he says.
3D ultrasound systems developed in Fenster’s laboratory have been patented and licensed to multiple companies. With rates of liver cancer rising in Ontario and around the world, Cool and Fenster hope their system can help make thermal ablation more accessible, especially when expensive CT scanners are not accessible.
“We hope to make this procedure much more accurate and less variable, and potentially change the paradigm of how patients are treated in Ontario and around the world,” Fenster says.