Toronto researchers unravel key cancer-driving circuit between the “powerhouse” and the “brain” of leukemia cells, in big first step for future therapeutic discovery and development

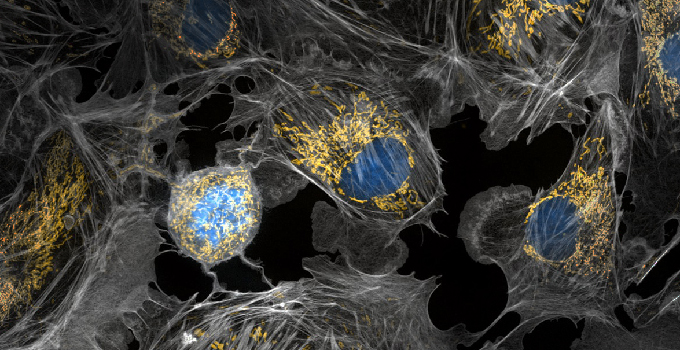
Over the last few decades, research has suggested that mitochondria, also known as the “powerhouses of the cell”, play an important role in tumour growth and development, but little is known about how to prevent these cellular machines from wreaking havoc. In a recent study, scientists have discovered a key protein that is made in the “powerhouse of the cell”, unexpectedly affects the expression of genes in the nucleus, or the “brain”, of certain leukemia cells. The study was launched by Dr. Dilshad Khan, who – alongside colleagues in Dr. Aaron Schimmer’s lab at the Princess Margaret Cancer Centre – set out to determine which genes in the mitochondria were essential to the growth and viability of acute myeloid leukemia (AML).
Through genome-wide CRISPR screening and other gene-manipulating techniques, they discovered a key mitochondrial protein that AML cells can’t survive without – MTCH2. Their findings, which were recently published in Blood, may eventually lead to new ways to fight this common and fast-growing form of blood cancer.
“We found that the mitochondrial protein MTCH2 is essential for the growth and survival of AML cells,” says Khan, Postdoctoral Fellow in the Schimmer Lab, who is the first author of the study. “But finding this protein was just one piece of the puzzle. We needed to understand how it worked.”
With Khan’s expertise in epigenetics, the team systematically dissected how MTCH2 affects AML cells. They found that blocking this protein would ultimately cause leukemic stem cells – the difficult-to-treat renewable cells that are thought to be at the root of leukemia – to irreversibly transform into cells that are easier to eliminate with existing chemotherapies.
“Through a series of experiments, we unraveled how MTCH2 affects AML cells and discovered that this protein has a remarkable and unexpected impact on nuclear pathways – it could control nuclear gene expression to affect AML stemness and survival,” says Khan. “We never thought this could happen, but now that we’ve discovered these new links, we could potentially find new ways to control these mechanisms.”
Next, the Schimmer Lab and collaborators plan to investigate MTCH2’s specific mechanism to find where inhibitors – or potential cancer drugs – could block its path. These initiatives will add to Schimmer’s research on dysregulated mitochondrial pathways in leukemia, including his recent work on fat production and copper distribution in leukemic stem cells. This research is funded in part by OICR’s Acute Leukemia Translational Research Initiative and OICR’s Cancer Therapeutics Innovation Pipeline.
“This study showed us that mitochondrial proteins are more interconnected with other cellular networks than we thought,” says Khan. “These fundamental findings have shed light on new research avenues that we can pursue to find new solutions that will hopefully benefit patients with AML.”