OICR’s PanCuRx program is unlocking the mysteries behind Canada’s fourth leading cause of cancer death and translating knowledge into better treatment options.
Tough to detect, quick to spread and stubbornly resistant to treatment, pancreatic ductal adenocarcinoma (PDAC) is one of the deadliest forms of cancer.
Most people won’t have symptoms in the early stages, giving pancreatic tumours — which can metastasize when they’re no bigger than a fingernail — plenty of chance to spread. By the time PDAC is detected, it’s often too late for surgery. Fewer than one in 10 people will live five years past their diagnosis.
But advancements in genomic sequencing have opened a new window into what makes PDAC so challenging. OICR led a major push to study and catalogue molecular data about pancreatic cancer that is generating key insights on how best to treat it. And OICR’s unique Pancreatic Cancer Translational Research Initiative (PanCuRx) is turning those insights into real-world treatment decisions.
“The way we’re applying knowledge in real time is very cutting edge and hopefully it can offer a better path for people with pancreatic cancer,” says Dr. Steven Gallinger, a surgical oncologist and PanCuRx co-lead.
Gathering and translating sequencing data
OICR’s work on PDAC dates back to the early years of the Institute when the International Cancer Genome Consortium (ICGC) was first amassing genetic data about different forms of cancer. As one of the founding organizations behind ICGC, OICR contributed whole genomes and transcriptomes (WGTS) from early stage pancreatic tumours, helping build the world’s first high-quality data set of PDAC genomes.
The data generated by OICR fueled pancreatic cancer research around the world and led to the launch of PanCuRx, a multidisciplinary OICR program led by Gallinger and Associate Director Dr. Julie Wilson dedicated to understanding PDAC’s molecular biology and translating knowledge into tailored treatment strategies.
PanCuRx launched the landmark COMPASS clinical trial in 2015 in collaboration with a clinical team at University Health Network led by Dr. Jennifer Knox. COMPASS aimed to show that pancreatic tumours could be sequenced and analyzed in time to influence a patient’s second-line care (after surgery or chemotherapy), potentially pointing them to treatment options that targeted their tumour’s unique biology.

This ambitious trial was not without its challenges. PDAC tumours are notoriously aggressive, so tumours had to be sequenced and analyzed quickly in order to have any meaningful impact on the next phase of treatment.
This was challenging because pancreatic tumours are difficult to sequence, both technically and logistically. Since the tumour biopsies were very small, with varying numbers of cancer cells, the PanCuRx team worked closely with UHN pathologist Dr. Sandra Fischer to implement a laser-capture microdissection technique to isolate and enrich the cancer cells which improved the quality of sequencing data. Multiple downstream steps were tightly coordinated so that the results could be discussed at a multidisciplinary ‘molecular tumour board’ to determine whether there were any molecularly guided treatment approaches that could benefit the patient.
Over five years and 270 participants, the trial successfully showed that genome sequencing could inform pancreatic cancer treatment decisions on a clinically relevant timeline. “That really made our mark in the world of translational research,” Gallinger says.
New insights to guide treatment
Proving feasibility was just one aspect of COMPASS. The sequencing and clinical data from the trial helped find clues about how PDAC responds to existing and potential treatment options.
For example, PanCuRx researchers identified four different subtypes of pancreatic cancer with distinct molecular properties that might be targeted by new therapies. They also found a rare mismatch repair (MMR) genetic signature that could make some pancreatic tumours more susceptible to immunotherapies.
One of the biggest discoveries was the GATA6 biomarker, which may be connected to how a pancreatic tumour responds to chemotherapy. GATA6 is still being validated as a biomarker through another clinical trial, but Gallinger says it is on the cusp on impacting treatment decisions. “It’s pretty convincing evidence,” Gallinger says. “If things go the way we expect, it could be influencing first-line care within a year.”
PanCuRx’s influence goes beyond its own trials. The huge amount of genomic data generated through the IGCG sequencing, COMPASS and subsequent trials is being harnessed by researchers around the world through the ICGC data sharing portal, the European Genome-Phenome Archive and other data repositories.
“I’m really happy to see our data shared widely and see so much good science is coming from it,” Gallinger says.
Driving collaborations across OICR
While collaboration with national and international scientists has been key to PanCuRx’s impact, some of the program’s most important connections are within OICR. “We’ve worked with colleagues in Diagnostic Development, Genomics, Informatics and all across the organization, and the teamwork has been amazing,” says Wilson.

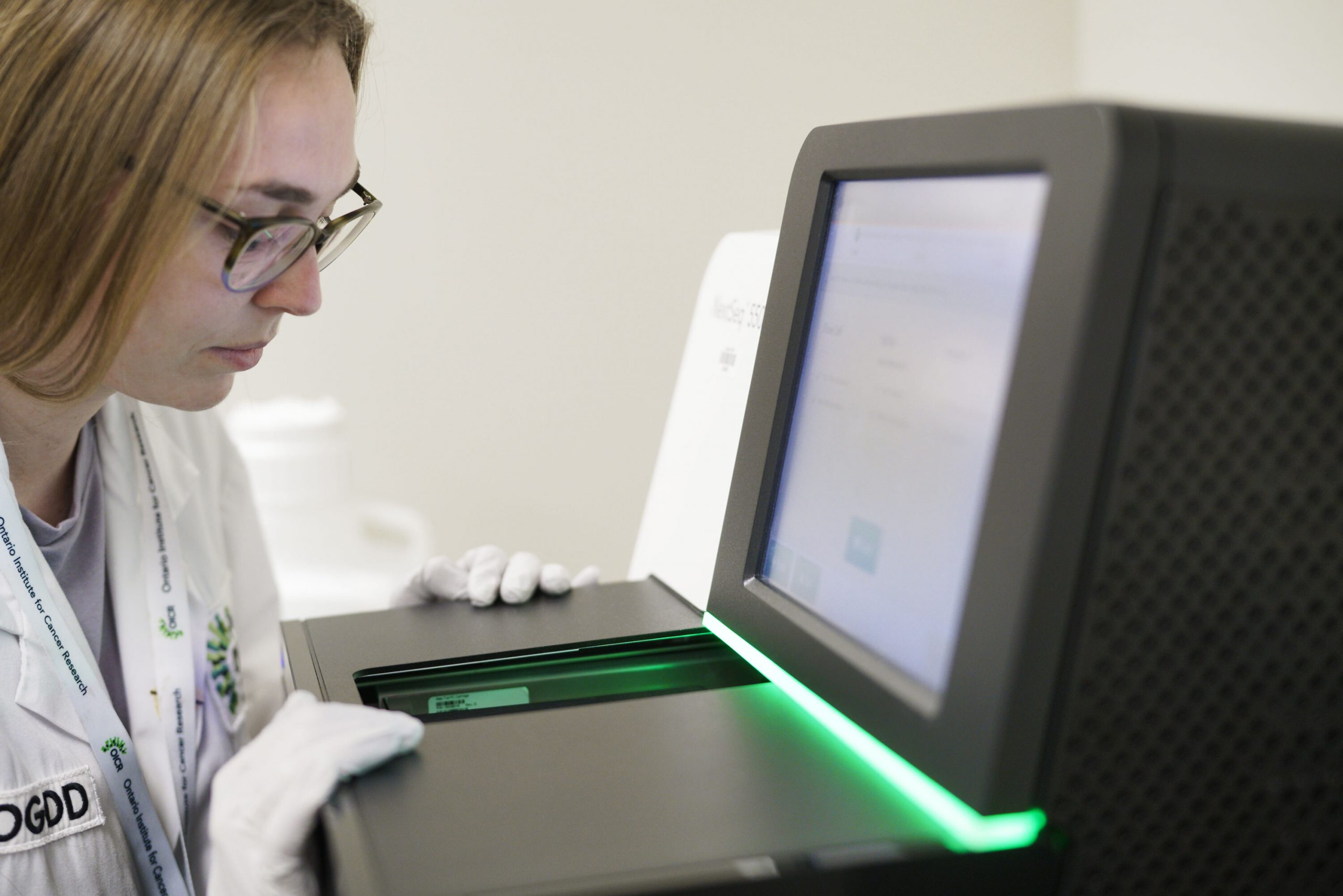
She says OICR’s genomics lab has played a particularly important role in PanCuRx work. In many ways, the two programs have evolved alongside each other, with OICR’s genome sequencing capacity growing to meet the needs of programs like PanCuRx.
One of the biggest evolutions came in recent years, when OICR Genomics earned high-level accreditation from the College of American Pathologists (CAP) and Accreditations Canada. This means that OICR Genomics’ sequencing reports can be used clinically — not just for research purposes — in the U.S. and Canada, which helps PanCuRx sequencing meet the tight turnaround necessary to influence patient care. “PanCuRx and OICR Genomics have a very symbiotic relationship, and it has helped make our program a leader in the field,” Wilson says.
Taking the next step to support patients
Already at the forefront of translational pancreatic cancer research, the PanCuRx team is ready to take the next step toward improving patient outcomes with the launch of the Provincial Strategy for Personalized Management of Pancreatic Cancer (Prosper-PANC) trial in summer 2022.
Like COMPASS, Prosper-PANC will see PDAC patients have their tumour’s DNA and RNA sequenced in the hopes of identifying new and existing treatments that target their unique form of cancer. But it will focus on a younger cohort of patients than its predecessors, capturing patients under 60 who tend to have more actionable mutations.
Prosper-PANC will also investigate other exciting innovations in precision medicine, including whether blood biopsies can be used to sequence pancreatic tumours, and whether patient-derived organoids (PDOs) can help identify targeted treatment options.
PDOs are three-dimensional clusters of cells generated from a patient’s tumour cells. When a tiny drop of a cancer drugs is added to the organoid, it tends to respond the same way an actual tumour would respond to the drug. “The jury is still out on how useful PDOs are clinically,” Gallinger says. “But the early data shows they mimic response pretty well for the standard cancer drugs.”
If Prosper-PANC once again shows that sequencing pancreatic tumours can help improve treatment strategies, the PanCuRx team hopes their model can be rolled out more widely across Ontario. With the trial set to run in Toronto, Ottawa, Kingston, and London, Gallinger says there is potential to scale it up.
“A year from now, if the evidence is even more convincing that sequencing can improve patient outcomes, we will find a way to make it more accessible to people all across Ontario,” Gallinger says.